Recently, I've been sharing some functional wellness tips on Instagram, so I thought I'd also post them here. If you are only here for the recipes, feel free to skip this one. However, you may want to skim the information really quickly because it could make all the difference in your health.
Functional vs. Conventional Medicine
I consider myself a functional medicine practitioner with conventional training. I've put in thousands of hours of training beyond my Registered Dietitian credential (which gives me a strong science foundation) to use a functional medicine approach with my clients. What is functional medicine?
The Institute of Functional Medicine defines it as
"Functional medicine is a systems biology-based approach that focuses on identifying and addressing the root cause of disease. Each symptom or differential diagnosis may be one of many contributing to an individual’s illness.
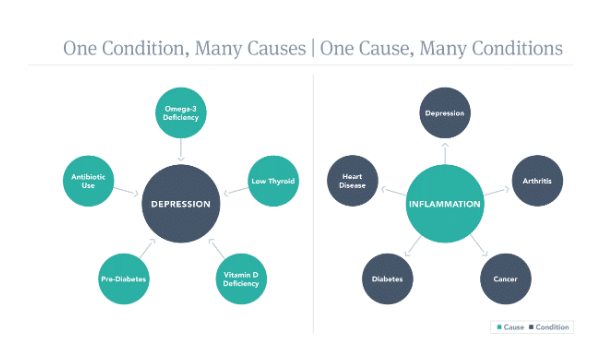
As the graphic illustrates, a diagnosis can result from more than one cause. For example, depression can be caused by many different factors, including inflammation. Likewise, a cause such as inflammation may lead to a number of different diagnoses, including depression. The precise manifestation of each cause depends on the individual’s genes, environment, and lifestyle, and only treatments that address the right cause will have lasting benefit beyond symptom suppression."
(I'm actually starting my IFM certification process in May! It's very expensive and has been on my bucket list for a long time, so I'm very excited! It will go towards my required continuing education as an RD)
Conventional medicine, on the other hand, generally models disease and treatment. Each disease process is typically looked at separately and each gets its own treatment. There isn't usually a "dig deeper" session. If you have depression, you can take an antidepressant; it's unlikely you could get a full workup of gut health, a full thyroid panel, Vitamin D, or consider a history of medication side effects.
I'm not a doctor. I can't prescribe medication, nor do I want to. I love being a Dietitian, here to support you, but not diagnose you. I can support your thyroid, reverse omega 3 and vitamin D deficiencies, help reverse pre-diabetes, and improve your gut health. I can also help you fight inflammation, lowering your risk of multiple types of illness. Sometimes I wish I had gone the naturopath route, but I think as a whole they often jump to supplements without really starting with diet and lifestyle focus first. I love that being a Dietitian I get to look at food FIRST as a primary mode of wellness. I'm actually part of a group of Dietitians in Integrative and Functional Medicine through the Academy of Nutrition and Dietetics.
True story: One time I had a family member of mine asking about a supplement for lack of smell/taste post COVID. This family member was on a number of supplements already but not taking care of their health. I explained that another antioxidant wasn't what they needed and may or may not help in their case. The olfactory nerve was inflamed, causing the lack of smell/taste, and the inflammation extended to the whole body. I listed off several other factors that pointed to lots of inflammation in their body. In other words, I refused to put another supplement in their account because they weren't doing anything else to take care of their health, so I felt strongly that the supplement was a waste of money. I'm happy to report my refusal sparked a two-year health journey where that family member started working daily, eating healthily, and managing their weight. I think a naturopath would have just given the supplement. But in my opinion, supplements are supportive of an already healthy lifestyle, not the other way around.
Optimal vs. Reference Ranges Blood Work
Optimal blood reference ranges are typically tighter ranges than reference ranges. Reference ranges on your bloodwork are somewhat controversial despite being used as the gold standard. In many cases, they are designed by the lab company, so they vary from company to company and are based on a sample population. They are set by determining whether 95% of healthy people in the sample population were within those ranges. It's safe to say the sample population, although not on their deathbeds, is likely not the picture of optimal health. I mean, 90% of the people in my life are not what I would consider optimally healthy, some more so than others, but still.
Instead, an optimal range is an evidence-based range where the lowest risk of disease and mortality may occur. Basically, where research says someone should be to prevent the progression of disease. So, in conventional medicine, if you are outside the range, they give you a medication. In functional medicine, if you're outside the optimal range but within the conventional range, we target that marker to improve it, hopefully preventing your progression to need medication. This is usually done with a combination of nutrition, lifestyle, and supplement support. Nothing crazy, just good prevention techniques.
Your doctor may say your bloodwork is normal, but when I get my hands on it, I might see a lot we can work on together to keep you healthy.
7 Blood Markers With Optimal Ranges You Should Pay Attention To
While every blood marker technically has an optimal range and conventional range, there are six that I pay special attention to that I wanted to share today. I'm identifying these six because they have a major impact on health when outside the optimal range, even when they are still within the conventional range. If I see these outside of optimal, I target them. Partially because they are low-hanging fruit, they respond well to nutrition and lifestyle intervention, and because the evidence is strong that the optimal range is more ideal.
1. Vitamin D
Vitamin D has far-reaching effects on the body as it's a vitamin that acts as a prohormone. In reality, there isn't anything that Vitamin D doesn't touch, from immune function, bone health, pregnancy/fertility health, inflammation, mood regulation, sleep cycles, and cardiovascular outcomes. There is strong research that shows that 50 is the minimum sufficient level for most people despite the cutoff in the reference range. Significant research evidence suggests that being over 80 may be excessive.
The reference range is > 30 ng/mL.
Optimal range 50-80 ng/mL.
In this case, if we are outside optimal, we increase Vitamin D in the diet and utilize supplements to get into the range.
2. TSH - Thyroid Stimulating Hormone
TSH, or thyroid stimulating hormone, is a marker I've been discussing a lot on Instagram recently. This is a screener thyroid panel that is typically standard on yearly bloodwork. This hormone is produced by the pituitary gland and signals when something is off with the thyroid. If the thyroid isn't producing enough of its own hormones, TSH will rise to nudge the thyroid. If it's producing too much, TSH will lower to calm things down. The reference range is HUGE on this one, and research suggests that a tighter reference range is indicated to identify subclinical thyroid dysfunction or sometimes outright thyroid dysfunction.
The reference range is 0.45 -4.12 mIU/mL
Optimal range 0.5 - 2.5 mIU/mL
In this case, if we are outside of optimal, I want a full thyroid panel to see how the rest of the markers are looking. Then, we will start to look at all the nutrition deficiencies, diet, and lifestyle choices that we can implement to protect the thyroid from progressing to outright dysfunction. However, I've seen clients with an unoptimal TSH go on to be diagnosed with Hashimoto's or outright thyroid dysfunction, needing to be treated with medication, even though their TSH was in the conventional range.
3. Triglycerides
Triglycerides are another one I pay special attention to. Triglycerides are consistently linked to metabolic dysfunction, diabetes, and cardiovascular outcomes. I care way more about triglyceride levels than I do about cholesterol levels. However, it's also fuel, and too low levels would be a red flag for malabsorption, especially if I saw a client with tons of GI issues coming in way too low.
The reference range is typically 0-150 mg/dL
Optimal range is 70-100 mg/DL
Typically I see many clients between 100-150. This is one of the scenarios where we can implement dietary change and supplement support that will push them into the optimal range and halt metabolic and cardiovascular disease progression before it becomes a problem.
4. Fasting Blood Glucose
Fasting blood glucose is the marker, and my eyes immediately jump, too. Many of my clients are coming to me for weight loss, hormone imbalance, or gut health issues. If their blood sugar is doing funky things, I want to address it immediately. Fasting blood glucose outside of the optimal range indicates the development of potential inflammation or insulin resistance. I take this in context with hemoglobin A1c.
Reference range 65-99 mg/dL
Optimal range 75-86 mg/dL
If this and Hemoglobin A1c are outside optimal, we are going to work on it. If HbA1c is normal, then the FPG may have been a one-off. Have you been extra stressed the morning of the test, or something else raised your blood sugar the morning of the test, but it's not reflective of the past few months?
5. Hemoglobin A1C
Hemoglobin A1c is a 3-month rolling average of your blood glucose levels. I look at this in conjunction with the fasting blood glucose for the same reason as FPG (see above.)
Reference Range: 0 - 5.7%
The Optimal Range: 4.6 - 5.3%
If this is outside optimal, we are going to work on it. Blood sugar dysregulation needs to be addressed as it's a symptom of inflammation and insulin resistance. This directly affects metabolic function, hormone balance, and thyroid health.
6. Iron Panel/Ferritin
Oh man, I've been personally victimized by this one. I used to be cold all the time, bruised easily, and generally felt like a death in my workouts. I also hadn't had a period in many years. Even though my iron panel looked normal, my ferritin stood out to me. My ferritin was 22, and the cut was 9. It should be normal, right? I had recently learned that the optimal range may be greater than 50 or even 100. I supplemented, and not only did my period finally come back around that time, but the cold intolerance, easy bruising, and fatigue disappeared within a week. It was wild. If you have symptoms of iron deficiency but your panel looks "normal," you may want to re-evaluate this marker. Careful iron supplementation can be toxic even at lower levels, so you'll want to work with a health professional on this one to bring your levels back to adequate. Also, thyroid dysfunction and iron deficiency symptoms are similar, so you'll need to tease out which one you truly have.
Reference Range Range: 16 - 232 ng/mL (16 - 232 ug/L)
Optimal Range: 50 - 79 ng/mL (45 - 79 ug/L) *Optimal may vary depending on cycling status or gender.
7. CRP
CRP is one of the most well-respected markers of inflammation. Except in acute illness, inflammation is generally not great for the body. So, based on research, I want this number in a tighter range to ensure the lowest levels of inflammation possible.
Reference Range: 0.00 - 7.9 mg/L (0.00 - 75.24 nmol/L)
Optimal Range: 0.00 – 3.0 mg/L (0.00 – 28.57 nmol/L)
Note - while these blood markers are important to look at. I'm looking at bloodwork, not to improve one marker overall unless it's a deficiency, then yes, we are trying to fix a deficiency like iron or vitamin D. But otherwise, we are looking at bloodwork to see what systems we can support. Thyroid health, hormone balance, detoxification, insulin resistance/blood glucose metabolism, gut health? What will make the biggest impact on improving overall health? Remember, there are many causes for one disease or one cause, many diseases. It's systems-based; it's not a direct line but instead a whole-body root cause approach. And remember it's not conventional or functional medicine, western or eastern, it's BOTH. I whole heartedly believe we need both.




aaradhanatechnology says
nice