This has been the year of functional and integrative lab training for me. I’ve completed over 100 hours of training in hormone balance and gut health, two areas I’ve always been very passionate about. At the advice of a colleague of mine who is both a chiropractor and a dietitian, I decided to round out the end of this year with training on the GI MAP stool analysis test. Today, I want to share why I believe this test to be so valuable, who will benefit the most, and what you can learn from stool analysis testing such as the GI MAP.
What is a GI MAP?
The GI MAP is a stool analysis test that maps out the health of your gut microbiome, immune system health, and digestive functioning capacity. The best part about this test is that it gives you a pathway to personalize gut health protocols to get the best results for YOU. There are so many “gut health” protocols, and sometimes symptoms can help point us in the right direction of which supplements and lifestyle interventions might help. However, with the GI MAP, you don’t have to guess. The protocol can be personalized precisely for your needs, and you can retest to track progress (if desired.)
What does the GI MAP test for?
The GI MAP is broken down into nine sections (and 19 total subsections) :
- Pathogens (bacterial, parasitic, viral)
- H. Pylori & virulence factors
- Commensal and Keystone Bacteria (Phyla)
- Opportunistic/Overgrowth Microbes (dysbiotic and overgrowth bacteria, commensal and overgrowth, autoimmune and inflammatory)
- Fungi/Yeast
- Viruses
- Parasites (protozoa, worms)
- Intestinal Health Markers (digestion, GI, Immune, Inflammation)
- H. Pylori Antibiotic Resistance Genes
What can you learn from each of these sections?
Pathogens
Pathogens can cause gastroenteritis leading to uncomfortable IBS-type symptoms like diarrhea, bloating, and even vomiting. Here is the thing that I find the most interesting about this section. You’ll note that many of these are organisms you may have heard of, particularly C Diff, which is often a hospital-acquired infection. Usually, these pathogens will be treated with aggressive antibiotics when symptoms are VERY severe. But sometimes, these pathogens can colonize (or recolonize after an infection looks clear) on a lower level. They cause fewer severe symptoms (so you probably won’t go to the ER), but you will likely be uncomfortable and symptomatic. You may blame your symptoms on food sensitivities, eating out, or stress, but these pathogens could hang around and be the true culprits of your symptoms.
- Bacterial and Related Toxins: E.coli, salmonella, C.diff
- Parasitic: Cryptosporidium, Entamoeba histolytica, Giardia
- Viral: Think adenovirus or norovirus
What if you test positive for one of these? I give my clients two options. Head to their GI doc or GP for conventional treatment with antibiotics. Or, if they would rather, they can use an all-natural “kill” protocol with supplements and essential oils to get rid of these from your gut without putting your microbiome through the stress of antibiotics. There are pros and cons to conventional and natural approaches that I talk through with my clients to help them make the best choice for them.
H. Pylori and Virulence Factors
H. Pylori is associated with gastritis, peptic ulcers, and stomach cancer. Some people, maybe up to 50% of the population, are asymptomatic carriers. But, even for those who are asymptomatic, H. Pylori can opportunistically take over in periods of low immunity or high stress. H. Pylori is also known to co-exist with other opportunistic microbe overgrowths (such as strep) and produces an enzyme, urease, which lowers stomach acid. Stomach acid is crucial to a healthy, functioning digestive system. You need ample stomach acid to kill pathogens that make their way to the stomach, digest proteins effectively, separate essential micronutrients (such as iron and vitamin B12) from proteins for absorption, trigger the release of digestive enzymes, and trigger proper emptying of the stomach contents into the small intestine (which is how low stomach acid can cause GERD).
H. Pylori strains produce virulence factors to help them survive. Specific factors are correlated with particular human health responses. We can target and support if any of these are present.
What if you test positive for H. Pylori? I give my clients two options. Head to their GI doc or GP for conventional treatment with antibiotics. Or, if they would rather, they can use an all-natural “kill” protocol with supplements and essential oils to get rid of these from your gut without putting your microbiome through the stress of antibiotics. There are pros and cons to conventional and natural approaches that I talk through with my clients to help them make the best choice for them. Particularly with H. Pylori, it can be difficult to eradicate with either approach. We also support digestion if we see patterns of H. Pylori causing low stomach acid (see GI Map Patterns section below). I also recommend an oral health protocol as H. Pylori can colonize in the mouth, and we discuss partner treatment/testing as H. Pylori is highly contagious.
Commensal/Keystone Bacteria
These are the good guys! We want to ensure you have an adequate and diverse population of these bacteria because they reduce the likelihood that less favorable bacteria will have a chance to overgrow. They produce nutrients such as short-chain fatty acids and vitamins. They also support the integrity and health of the entire GI tract (literally, think how healthy the actual tissue that makes up the GI tract tubes are.) They are also known to be immune system supportive and anti-inflammatory.
However, because of antibiotics and other gut-depleting chemicals in our environment, many people have a low-functioning or wiped-out gut microbiome, and their off-the-shelf probiotics aren’t even making a dent in reinoculation.
What if you are low? We will reinoculate with high-dose probiotics explicitly chosen based on your results and, depending on which strains you are low on, potentially add fiber supplements to support reinoculation. We also may need to replace nutrients produced by certain strains that are low while you reinoculate.
Opportunistic and Overgrowth Bacteria
Some of the bacteria in this category can be normal findings in the GI tract. However, if allowed to overgrow, they can cause many symptoms. Some of them are related to autoimmune conditions and inflammation in the GI tract.
What if you test high? We use an all-natural “kill” protocol with supplements and essential oils to remove these from your gut without putting your microbiome through the stress of antibiotics. If you are low in keystone bacteria, reinoculation with good bacteria will also help lower these less favorable strains.
Fungi/Yeast
Like the above, fungi/yeast findings can be expected in the GI tract. However, because of the extensive use of antibiotics and gut microbiome-depleting environmental toxins, yeast/fungi can become overgrown. In those cases, an overgrowth can cause many symptoms extending well beyond the GI tract. Think autoimmune, hormonal, and more.
What if you test high? I use a natural protocol here as well. This protocol will also extend to a specific dietary protocol low in sugar and starch to help kick the yeast/fungi, which often feed off sugar. I may occasionally refer out and recommend pursuing conventional antifungal treatments for very high levels or persistent cases. This is on a case-by-case basis. But, sometimes, antifungals are appropriate and have far fewer side effects than antibiotics.
Viruses
This section will only be positive if you have an active infection. You will be referred to a primary care physician if you test positive.
Parasites
This section will only be positive if you have an active infection. If you test positive, you will be referred to a primary care physician, as they will require conventional treatment to eradicate. Since conventional medicine tests for these parasites when symptoms warrant the tests, it’s unlikely someone doing a GI Map would test positive, but it is possible.
Intestinal Health Markers
The GI Map tests for seven intestinal health markers in four sections.
Digestive Health Markers
Steatocrit – 1 – a measure of fat in the stool, tells you how well you are breaking down and absorbing fat from your food. We want this to be as low as possible. When high, we will relate this to pathogen or bacteria overgrowth that could contribute to it. We will support proper digestion while trying to get to the root cause of why this might be high. Common causes include hypochlorhydria, maldigestion, malabsorption, pancreatic insufficiency, bile salt insufficiency, improper mastications, and celiac disease.
Elastase -1 – a digestive enzyme secreted exclusively by the pancreas, directly indicating pancreatic function. Elastase 1 is unaffected by pancreatic enzyme replacement therapy. There are several reasons why this might be low, including decreased pancreatic output, hypochlorhydria (especially if H. Pylori is present), cystic fibrosis, gallstones, and a vegetarian diet. We will want to support optimal stomach acid and digestion through various tactics, such as replacing acid, bile salts, and enzymes. (Not all these treatments are used for every client, it’s on a case-by-case basis.)
GI Markers
Beta-Glucorindase – an enzyme produced by bacteria and the intestinal cells that, while necessary for carbohydrate metabolism, at high levels, is associated with colorectal, breast, and prostate cancer. If levels are high, we will support the liver (as beta-glucuronidase undos the detox process of glucuronidation in the liver.) If constipation is also present, we will likely start our protocol with a detox month. We will also make dietary changes (including foods known to lower beta glucorindase and macro distribution) and supplement protocols to reduce this number.
Occult Blood – FIT – the presence of blood in the stool is an important marker. No specific protocol action is taken on my part, except for recommending to retest to ensure it goes away and, depending on age/history/etc., maybe a referral to GI for colonoscopy if one wasn’t done recently.
Immune Response
Secretory IgA – a measure of overall immune function and immune health in the gut. When this number is high or low, actions will depend on why we think it’s high or low. Such as long-term infection vs. acute infections, etc. In low cases, immune and gut permeability support is warranted.
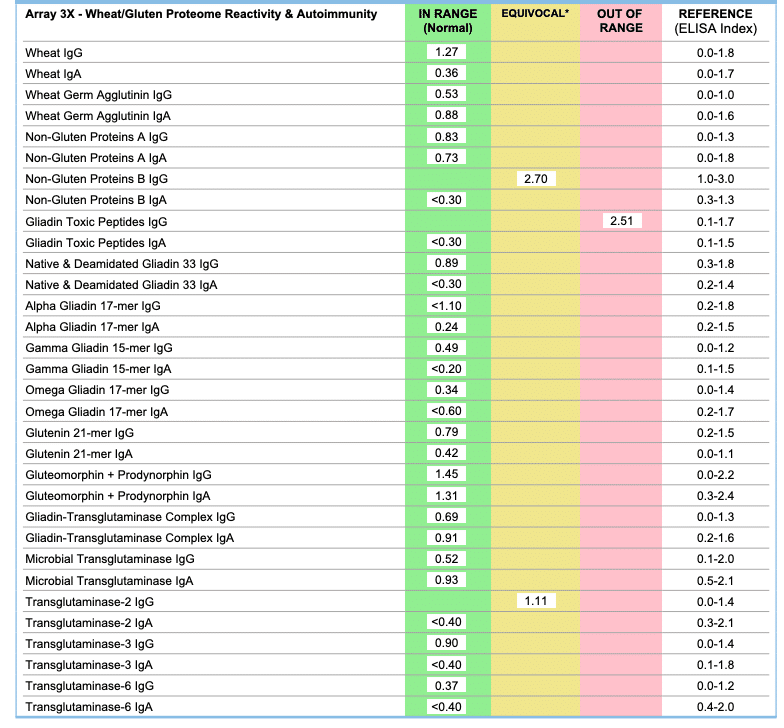
Anti-Gliadin IgA – a measure of antibodies being produced to wheat/gliadin/gluten products in the gut. Stool antibodies don’t always correlate with those found in the blood. Although, it’s arguable that high-level GI tract production warrants removing gluten from the diet. However, if I see this high, as we did with Mr. Hungry, I would recommend running a Cyrex Array 3X Wheat Screen and maybe a celiac genetic screen. That way, we know whether your reaction is systemic or localized to the GI tract. We did this with Mr. Hungry, and he did have reactions to wheat components in the blood, so he is now gluten-free. (I don’t love to give out gluten-free diets willy-nilly, especially in my own household. It’s expensive and inconvenient. But his decision to go gluten-free was fueled by his own results and by a family history of autoimmunity and one of his parent’s 3X tests that lit up like a Christmas tree – very reactive to wheat. Even though, as you can see below, he only has a couple of markers out of range.)
GI MAP results –>
Follow Up Cyrex Array 3X Blood Test Results for Mr. Hungry –>
Eisophil Activation Protein – a protein released by eosinophils that play a role in inflammatory and mast cell-mediated pathologies. There are several possible causes, and treating the underlying root cause is the most important factor if this number is high.
Inflammation
Calprotectin is a well-known inflammation marker and strongly correlates with risk or current inflammatory bowel disorders, inflammation, infection, food allergens, polyps, diverticulitis, and colorectal cancer. If you are high, we will want to treat any underlying reasons (high gliadin antibodies, infections, etc.) and support you with anti-inflammatory supplements.
Add-On Tests – Zonulin
Zonulin is a protein that opens tight intercellular junctions in the gut lining. It’s a biomarker for a leaky gut. However, there is some controversy about whether this marker is actually diagnostic for leaky gut. My preferred leaky gut test is the Cyrex Array 2 Gut Permeability Screen, which looks at antibody production to zonulin. Suppose you have antibody production to a normal protein found in your gut. In that case, you can be reasonably confident that the protein is “leaking” through the gut barrier (along with other food particles and toxins), creating a systemic reaction. Therefore, for my clients who are concerned about leaky gut or fit the profile, I would skip the add-on zonulin and do the Cyrex test concurrently with the GI MAP from Diagnostic Solutions. However, this decision would also be dependent on budget and symptoms.
5 Common GI MAP Patterns
- Dysbiotic Insufficiency – in this case, the healthy gut bacteria are just not optimal in variety or numbers. The main goal here is reinoculating the GI tract. This pattern was pretty clear on Mr. Hungry’s test.
- Inflammatory Dysbiosis – in this case, we see several inflammatory opportunistic overgrowth microbes and potentially elevated intestinal health markers of inflammation.
- Digestive Dysfunction Dysbiosis – a commonly observed pattern typically associated with H. Pylori and other co-infections resulting in low stomach acid, insufficient bile acids, poor digestion, and altered gastric motility.
- Immune-Mediated Food Reactions & Leaky Gut – An overgrowth of histamine or mast cell-producing bacteria and elevated intestinal health markers can signal that the root problem of symptoms may be a leaky gut. We need to test gut barrier function with leaky gut testing and potentially look at food sensitivity testing for complete healing.
- SIBO Patterns – an overabundance of Gas and histamine producers on the GI Map results coupled with symptoms of gas and bloating.
Who Benefits From a GI MAP Test
I believe anyone could do this test and get value from it. But, unless you have Medicare or can reimburse through your HSA/FSA, you are likely paying out of pocket for it. Plus, you’ll need a review appointment and supplement protocols to correct imbalances. So, although Mr. Hungry and I will likely be redoing our GI MAPS every couple of years (at least while we have preschoolers bringing home all kinds of things requiring antibiotics at least two times a year) for preventative wellness (this and the DUTCH test I find highly valuable), I wouldn’t suggest it to a client for that reason unless they asked, because again, out of pocket costs can add up fast.
Here are some scenarios where I might suggest utilizing the GI MAP:
- Gastrointestinal distress
- Bloating or Gas
- Diarrhea and/or constipation
- GERD
- Autoimmunity
- Weight loss resistance
- Depression or anxiety
- Past infections such as Lyme or heavy use of antibiotics
- Hormone imbalances
In each case, the GI MAP test may or may not be the first-line test I recommend. For GERD, I think stool analysis is the best bet. And for weight loss resistance, it can be helpful. But it would likely be a second-line test for some of these other conditions, such as PCOS or fertility.
Pros and Cons of the GI MAP Test
Pros
- GI MAP is easily collected at home and is not an invasive test.
- It’s lower cost than other stool analysis companies. In fact, medicare part B will cover it completely.
- It gives you a personalized gut health protocol that you don’t have to guess at.
- Gut health is a “root cause approach to health,” meaning instead of fixing your symptoms, and it improves the root cause of a whole host of ailments. The gut microbiome is related to immune, hormonal, neurological, endocrine, and metabolic functions.
Cons
- It’s an out-of-pocket expense for some people, although this varies by the insurance company.
- Stool analysis is not perfect. Sometimes, you can test negative for microbes that are there because they just weren’t shed in that sample. (Some other than GI MAP companies offer 3-day analysis, which helps lower this issue but at a higher cost. I will review those options in upcoming posts.)
- You don’t always need to test. Sometimes, we can get pretty far with the functional Fab Five supplements and a gut-healing protocol diet.
If you are interested in getting a GI MAP test and working with me to review it, you have a couple of options:
- Sign up for a GI MAP package, which includes the test and the review appointment. This comes with a personalized list of supplements, my gut health diet program, and more lifestyle recommendations to improve your gut health.
- Sign up for a gut health-centered package with six months of nutrition counseling. (Releasing these in a few months, but you can find out more here.)
- Sign up for a consult. The consult cost will go to whatever package we decide is best for you, including nutrition counseling or anything else.
- Email me with any questions or special scenarios. For instance, if you want to use Medicare to pay for the test or aren’t sure where to start.



[…] Is A GI-MAP Test Worth It?: Diagnostic Solutions Lab, Nikki Yelton RD, Ann Arbor Holistic Health, Hungry Hobby, Dr. Chris Jones, Dr. Laura […]